The Interventional Radiology team at Rochester Regional Health offers the full spectrum of minimally invasive interventional treatments for liver cancer, including Y90 radioembolization (as well as other procedures such as chemoembolization and ablations).
Y90 radioembolization is a minimally invasive procedure allows the direct delivery of tiny radioactive particles directly into liver tumors, destroying cancer cells from within the tumor while minimizing the damage to surrounding tissue.
Tumors are not always cancerous, but even benign (non-cancerous) tumors can cause problems when left unchecked. Radioembolization Y-90 (which stands for Yttrium-90 embolization) is a minimally invasive treatment for primary or metastatic liver cancer that combines radiation therapy with embolization.
During a radioembolization procedure, the interventional radiologist places tiny glass or resin beads filled with the radioactive isotope yttrium Y-90 inside the blood vessels feeding your liver tumor. They block the cancer’s blood supply and deliver a high dose of radiation to your tumor while sparing normal, healthy tissue.
Your radioembolization is performed entirely through a tiny nick in your skin, and you will be able to return home mere hours after the procedure.
Y90 radioembolization is a treatment for patients who have predominantly liver tumors and who are not good candidates for surgical removal.
Although originally FDA-approved for liver metastases spreading from colon cancer, it has been approved and is used for numerous other cancers which originate or spread to the liver. The most common cancers treated by Y-90 include metastatic colorectal cancer, hepatocellular liver cancer (HCC), and neuroendocrine liver metastases.
For many patients, this type of treatment is not meant to be curative; treatment goals include local disease control, downstaging to allow for surgery, bridging to transplantation, and extending survival. For certain patients in the correct setting, this may be curative.
You can either call our office and schedule a consultation for yourself, or you can have your oncologist help set you up. At your appointment, you will meet with the interventional radiologist (IR) who will perform your procedure. First, we will ask about your history and background. It is very important for us to know what chemotherapy and radiation treatments you have previously undergone, and when. If you are deemed an appropriate candidate, the procedure and background are explained in depth, and a discussion is had to determine if this is the correct procedure for you. All of your questions will be answered, and you will receive literature to help you understand this treatment.
Prior to your procedure, your blood will be tested to determine how well your kidneys are functioning and whether your blood clots normally. You will also have a special type of CT known as a CTA or CT Angiogram. This CT shows us the extent of your tumor, allows us to accurately analyze the size (volume) of tumor, and allows us to map out the anatomy of your vessels.
If you are deemed an appropriate candidate for radioembolization after your consultation, we will discuss the plans for treatment with your other cancer doctors and then schedule treatment days that are convenient to you. The procedure takes place on two or three separate days, depending on your tumor and overall health.
Day one involves mapping your angiogram and shunt embolization–this can be considered a “test run”. Weeks later, the subsequent procedure day(s) entail the actual injection of the Y90 radiation particles into your liver. Only one half of the liver is treated at a time, and those who need injections on both sides may return for two procedures. None of the procedures typically last longer than 90 minutes, and patients almost always return home on the same day.
There are two separate steps/procedure days associated with radioembolization:
Step 1: Mapping Angiogram and Possible Shunt Embolization
This is a preparation day before the actual treatment to make sure the radioactive particles go to the tumor sites. Once you arrive in the interventional radiology holding area, you will be prepped by your nurses for the procedure. Your mapping angiogram and shunt embolization take place in a room called an interventional radiology suite, which looks very similar to the operating room. There will be a large C-shaped machine next to the bed, which allows us to shoot the equivalent of movies once contrast is injected (your angiogram).
You will be moderately sedated, a type of sedation that uses a combination of medications to make you feel sleepy and drowsy while also minimizing pain. Although it will be possible to rouse you, most patients tend to sleep or remain drowsy throughout the procedure. We need you to stay rousable so that you can hold your breath for the few angiograms we perform, otherwise we would take a blurry “movie” due to the breathing motion. Once you are sedated, your interventional radiologist will numb the skin in your groin with lidocaine and gently insert a catheter into the artery before carefully advancing it towards your liver.
We will take multiple angiograms, which act like maps of your blood vessels leading to and inside the liver. At this point, it is critical to block any extra pathways (using shunts) that could potentially allow the radiation particles to travel in a non-target direction back towards your stomach. Blocking these shunts is called embolization.
After your shunt embolization, your interventional radiologist will inject particles to do a test run. Once your particles are injected, you will have a “perfusion scan,” to show if most, if not all, of the particles are staying in the liver and not accidentally traveling elsewhere. This is a crucial step, because unwanted particles in your stomach can cause severe ulcers and bleedings, while unwanted radiation particles in your lungs can cause radiation fibrosis.
Step 2: Y-90 Radioembolization with Particle Delivery
Once we’ve completed your mapping angiogram and shunt embolization, we will know for sure if it’s safe to inject the Y-90 particles. You will be called within a few days to schedule the actual Y-90 injection days.
These days are generally much quicker than the mapping angiogram days. After you’re sedated, a catheter will be placed in the arteries leading towards your tumor(s). The radiation-filled microspheres, or resin beads, are then slowly and carefully injected through a microcatheter into the arteries feeding the tumor.
Once the microspheres are lodged at the tumor site, they deliver a high dosage of radiation directly to the cancer cells. This allows us to deliver higher doses of lethal radiation to your tumor while sparing surrounding healthy tissue. The microspheres will block the flow of blood to the tiniest vessels in the tumor, depriving the diseased cells of the oxygen and nutrients needed to grow. The radiation will continually decrease over a two-week period and disappear after 30 days, while the tiny microspheres will remain in the liver without causing any problems.
Radioembolization is generally tolerated quite well, but some patients may experience brief pain when the microspheres are injected. The procedure is usually completed within 90 minutes, and usually is conducted on an outpatient basis.
Patients typically experience mild side effects called post-embolization syndrome, including nausea, vomiting, abdominal pain and cramping, and fever. Weakness, low grade fever, malaise, and fatigue are the most common side effects that occur and are actually expected.
This typically lasts about one week.
You should be able to resume normal activities within a day or two following the procedure. However, during the week following your radioembolization, you will need to limit contact with others while the radiation in your body diminishes. You should not do the following for at least seven days after the procedure:
CT scans or MRI may be performed every three months following the treatment to determine the size of the treated tumor.
Chemoembolization is a minimally invasive procedure performed by an interventional radiologist that directly targets tumors in the liver. It is similar to Y90 but works on slightly different principles. It works by dual but complimentary means, first injecting chemotherapy directly into the tumor, and then stopping the blood supply to the tumor.
This double-injury method causes cell destruction of the tumor while sparing normal liver tissue and reducing side effects of chemotherapy elsewhere in the body. Sometimes, a third injury technique is added for certain cases, in which the tumor is also ablated using either a freezing (cryoablation) or heating (radiofrequency ablation) method.
You will initially come in for a consultation in our Rochester Regional Health Interventional Radiology office to fully discuss the problem and all the treatment options to ensure that this is the right treatment for you. Prior to your procedure, labs and a special type of CT called a CT angiography will be performed to evaluate and map the tumor and all the arteries leading to it.
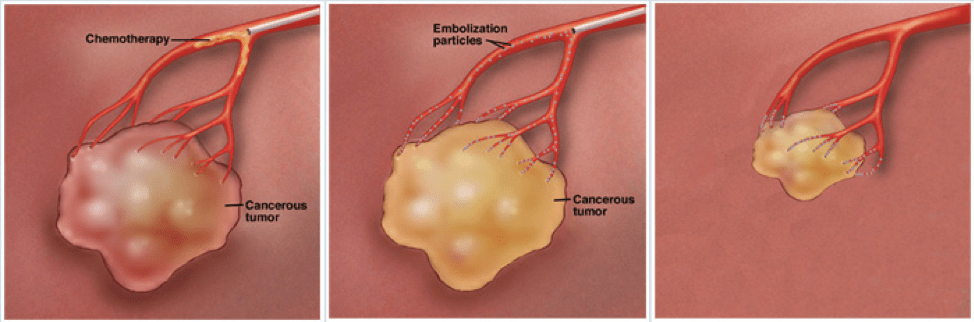
On the day of the procedure, you will be prepped in the pre-procedure area and brought to the interventional radiology suite. Under local anesthesia, a tiny catheter (tube) is introduced into an artery in the groin and advanced under image guidance into the livery artery that feeds the tumor. There, tiny particles – smaller than grains of sand – are released. These tiny particles have a specific chemotherapy attached to them tailored to the specific type of tumor. These particles are then preferentially taken up by the liver tumors which tend to steal the normal liver blood supply.
Chemoembolization has become a mainstay of liver tumor treatment over the past 30 years. The procedure usually takes less than 1-2 hours, is performed with conscious sedation rather than general anesthesia, and usually only requires an overnight stay for observation.
Chemoembolization is a minimally invasive procedure, with no surgical incision, therefore greatly reducing the time needed for recovery. Recovery from the catheterization usually involves 4 hours of bedrest in the recovery area keeping the legs straight. Recovery for the chemoembolization of the tumor usually involves overnight observation for post-embolization syndrome. This includes abdominal pain and cramping, nausea, fever, and malaise. Many patients state that this recovery, which usually only lasts overnight, is similar to the flu.
We keep patients overnight to ensure they are comfortable and provide any medications that they may need until the post-embolization syndrome resolves. The chemotherapy delivered is focused int the tumor, so the side effects are often much less when compared to when chemotherapy is given into the entire body (systemic chemotherapy) to fight cancer.
The risks of the chemoembolization include risk of bleeding, clot, and infection. Non-target embolization refers to particles being injected into an unintended area, but is rare if being performed by an experienced physician. Liver failure is also a possible complication, which is why labs will be drawn and full medical history explored during your initial consultation to ensure you are a proper candidate.
Finally, our IR division also has an active tumor ablation program. This treatment is different than Y90 and chemoembolization is that, simply put, tumor ablation is a procedure where ultrasound or CT imaging is used to place a probe directly into the tumor. If you have had a biopsy, this process of placing the probe is nearly identical.
Then, while the patient is sedated, the tumor is either burned (microwave ablation or radiofrequency ablation) or frozen (cryoablation) in order to destroy the cancerous cells as well as get a clear margin around the tumor. Location, size, and type of tumor all play into the decision-making as to whether ablation or Y90 or chemoembolization will work best. The most common locations that we perform tumor ablation on are kidney tumors, liver tumors, lung tumors, and bone tumors.
